Healthcare organizations are in the eye of information overload storm. With EHR, EMR and with HIE implementation, there’s tons of data that will be available to payers, care providers and care management companies. The data latency will be reduced to days and in hours if not in minutes from weeks/months where is stands today. Healthcare organizations are rapidly adopting information systems to improve both business operations and clinical care. The need to reduce costs, the demand for improved quality, and significant change are three formidable, mounting pressures on healthcare. At the same time, healthcare organizations are adopting methodologies such as Lean and Six Sigma to take a more patient-centric focus, reduce errors and waste, and enhance patient flow with the goal overall goal of improving quality.
In healthcare, there is both a growing availability of and growing demand for accurate, timely, and readily available information throughout the organization and for different purposes. Sometimes identified as a branch of Business Intelligence, Analytics has been described as the “data, statistical, and quantitative analysis, explanatory and predictive models, and fact-based management to drive decisions and actions”. Not surprisingly, healthcare business analytics – the key to extracting valuable insights from all that data being collected-is in vogue. From 2007-2011, IBM spent more than $15 billion to acquire 26 analytics-related companies. Furthermore, the value of analytics to healthcare has become more evident, as James Cortada, Dan Gordon and Bill Lenihan of IBM observe: “Healthcare organizations around the world are challenged by pressures to reduce costs, improve coordination and outcomes, provide more with less and be more patient centric. Yet, at the same time, evidence is mounting that the industry is increasingly challenged by entrenched inefficiencies and suboptimal clinical outcomes. Building analytics competency can help these organizations harness ‘big data’ to create actionable insights, set their future vision, improve outcomes and reduce time to value.”
With the launch of ACO this Jan 2012, many large Health Plans and Care Management companies has been working towards their plan to evolve into ACO business. The ACO model requires providers along the continuum of care to share the responsibility for providing care to patients and take on risk together as one entity. Health plans can play an important role in ACOs because they track and collect data on patients, which is critical for coordinating care and reporting on the results. Health plans can play a critical roles in such initiatives by providing tools and data to support population based care, providing programs and staff to better coordinate care, and structure provider contracts to reward high quality performance and reductions in cost. While providers and health plans work on creating new reimbursement models to support these changes, provider care systems are finding an escalating need to have access to analytics derived from claims data.
ACOs over time will require a lot more I.T. firepower, including pervasive connectivity, data analytics and predictive modeling technology supported with robust disease, care and utilization management applications to support care across the continuum while identifying opportunities to reduce costs. Regardless of the pace that providers will launch their ACO initiatives, CIOs and I.T. departments already are overwhelmed with meaningful use, ICD-10, HIPAA 5010 and forthcoming enhanced privacy/security mandates.
As required by the Affordable Care Act, before an ACO can share in any savings created, it must demonstrate that it met the quality performance standard for that year. CMS will measure quality of care using nationally recognized measures in four key domains using 33 quality measures:
- Patient/caregiver experience (7 measures)
- Care coordination/patient safety (6 measures)
- Preventive health (8 measures)
- At-risk population:
- Diabetes (6 measures)
- Hypertension (1 measure)
- Ischemic Vascular Disease (2 measures)
- Heart Failure (1 measure)
- Coronary Artery Disease (2 measures)
However, the reporting of these measures is not trivial. It’s not a case of just writing a new report or an extract and sending it over to the CMS. There are numerous data collection, data quality, and data integration challenges that even the top IT departments have problems overcoming. Specifically, the healthcare data required to produce these metrics are often found in multiple disparate systems, stored in proprietary databases, or contained on numerous static reports, access databases and .pdf files that cannot be utilized for analytical purposes without analytics and BI toolsets. Attempting to overcome the data integration challenges of report data from several clinical systems, EMR’s, decision support applications, which are often in different formats, layouts, etc. is a daunting task – one magnified when you also realize that the required data needs to be integrated with data extracted from databases.
According to the Centers for Medicare & Medicaid Services, U.S. national health expenditure totaled $2.5 trillion in 2009, or $8,086 per person, and accounted for 17.6 percent of gross domestic product. Healthcare expenditures per capita are 2.4 times higher than that of other developed countries and are projected to increase 67.9 percent over the next ten years. Access concerns, such as the 45.7 million uninsured U.S citizens (15.3 percent of total population) are taking a toll on the healthcare system. In the recent IBM Global CIO Study, more than 90 percent of healthcare CIOs for top-performing organizations cited insight and intelligence as a key focus for their organizations over the next three to five years, compared to 65 percent of underperformers. Further, when these CIOs were asked about visionary plans to increase competitiveness, 83 percent of healthcare CIOs listed business intelligence and analytics as their top priority. Outperformers stretch the envelope and apply analytics in innovative ways that enable them to stand above their peers.
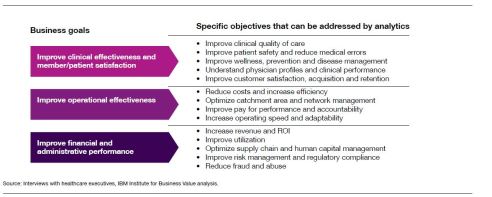
Beyond the general application of analytics to business goals, the development and use of analytics among top performers is geared towards achieving specific objectives and priorities. As below figure illustrates, analytics can be focused in a variety of ways to improve clinical quality of care, reduce costs and increase efficiency, and increase revenue and return on investment (ROI).
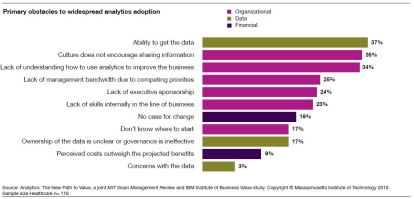
Many of the biggest barriers to analytics adoption are organizational. Here is the snapshot of top barriers based on a joint by MIT Sloan Management Review and IBM Institute of Business Value.
The healthcare industry is changing with incredible speed, and one of the major contributors to this change is the dramatic upsurge in healthcare communication brought on by social media. Not only has social media become a place where the public goes to seek health information, but by nature these social media channels allow for two-way public communication between patients, providers and other third parties, effectively creating the largest source of health discussions available globally today. This vast network of healthcare influencers, thought-leaders, patients, providers, organizations, and governmental entities daily create rich healthcare content, messages and signals that provide incredible value if it is segmented, analyzed and curated in a meaningful way to answer your unique questions and needs.
Another area where Healthcare Analytics has gain popularity is with fraud detection. The National Health Care Anti-Fraud Association (NHCAA) estimates conservatively that 3% of all health care spending—or $68 billion—is lost to health care fraud. Generally, healthcare frauds are not obvious and thus hard to detect. The followings are typical examples of healthcare fraud techniques used by health care providers and patients;
- Providers billing for services not provided.
- Providers administering (more) tests and treatments or providing equipment that are not medically necessary.
- Providers administering more expensive tests and equipment (up-coding).
- Providers multiple-billing for services rendered.
- Providers unbundling or billing separately for laboratory tests performed together to get higher reimbursements.
- Providers charging more than peers for the same services.
- Providers conducting medically unrelated procedures and services.
- Policy holders traveling long distance for treatment which may be available nearby. (Possibly scams by bogus providers.)
- Policy holders letting others use their healthcare cards.
Healthcare fraud detection involves account auditing and detective investigation. Careful account auditing can reveal suspicious providers and policy holders. Fraudulent claims often develop into patterns that can be detected using predictive models
The following techniques are effective in detecting fraud. Auditors should ensure they use these, where appropriate. They include the following:
- Calculation of statistical parameters (e.g., averages, standard deviations, high/low values) – to identify outliers that could indicate fraud.
- Classification – to find patterns amongst data elements.
- Stratification of numbers – to identify unusual (i.e., excessively high or low) entries.
- Digital analysis using Benford’s Law – to identify unexpected occurrences of digits in naturally occurring data sets.
- Joining different diverse sources – to identify matching values (such as names, addresses, and account numbers) where they shouldn’t exist.
- Duplicate testing – to identify duplicate transactions such as payments, claims, or expense report items.
- Gap testing – to identify missing values in sequential data where there should be none.
- Summing of numeric values – to identify control totals that may have been falsified.
- Validating entry dates – to identify suspicious or inappropriate times for postings or data entry
By leveraging the power of data analysis technology organizations can detect fraud sooner and reduce the negative impact of significant losses owing to fraud. Healthcare fraud is a serious financial drain on the health care systems in many jurisdictions. It represents a serious drain on the effectiveness of providing health care to those in need.
To be sure, the United States offers arguably the best healthcare in the world, but at what price? According to the American Journal of Medicine, medical bills capsized 62 percent of the people who went bankrupt in 2007. Clearly, healthcare in the United States can benefit from a strong dose of analytics to help improve the performance of a massive, complex, fragmented, hugely expensive system struggling to sustain itself.
References:
1) Davenport TH and Harris JG. 2007. Competing on Analytics. Boston: Harvard Business School Press.
2) “The value of analytics in healthcare.” IBM Global Business Services Executive Report, January 2012
3) Accountable Care Organization 2012 Program Analysis http://www.cms.gov/medicare/medicare-fee-for-service-payment/sharedsavingsprogram/downloads/aco_qualitymeasures.pdf
4) IBM Institute for Business Value. May 2009.
http://www-05.ibm.com/pl/public/pdf/Patient_centered_medical_home_White_Paper.pdf
5) The Essential CIO: Insights from the IBM Global Chief Information Officer Study. Healthcare Industry. IBM Institute for Business Value. http://public.dhe.ibm.com/common/ssi/ecm/en/cie03115usen/CIE03115USEN.PDF
6) Global Technology Audit Guide: Fraud Prevention and Detection in an Automated World. The Institute of Internal Auditors, 2009
About Encore Software Services:
Encore Software Services is a leading solution provider and systems integrator in Business Intelligence and Analytics domain. Our Analytics and Information Management services help customers accelerate business decisions by offering tailor-made comprehensive analytical solutions and frameworks. They are designed to enhance business performance by leveraging all forms of informational assets. Our solutions are customer specific to provide that added edge that our clients require for their business scenarios.
Encore provides an extensive suite of Analytics services that enable customers to mine this data and make analytical assessments. These services enable improvement in many areas such as customer support services, fraud detection in financial transactions, predicting success of new product offerings, context aware placement of Advertisements etc. Using industry standard tool sets combined with proprietary algorithms these analytic services use Big Data and Enterprise clusters to provide efficient processing of large data sets. You can visit us @ http://www.EncoreSS.com or reach us at spramanick@encoress.com.